1076
Views & Citations76
Likes & Shares
White spots or patches on newly erupted permanent incisors are common among young adolescents; this may cause aesthetic concerns for both the patient and the parents. Conventional treatment for managing this lesion is usually invasive. Resin infiltration technique is simple, conservative, and a generally well accepted procedure by patients. The material was introduced in the market to treat white spot lesions, enamel hypoplasia and for post orthodontic opacities. It is noticed that enamel lesions treated with resin infiltration have tendency to lose their whitish appearance as the porosities are filled with the resin. In this case series, we have demonstrated the successful use of resin infiltration (ICON®) for masking the white spot. The pleasing aesthetic results and the conservative nature of this approach makes it a good alternative to micro abrasion and conventional resin restorations.
Keywords: Minimal invasive, White spots, Resin infiltration, Micro abrasion
Abbreviations: WSL: White spot lesions
INTRODUCTION
Smiles are expression of emotions like happiness, love, joy and excitement. In a child, smile is sunshine. Sometimes with the eruption of permanent tooth, this smile fades to an embarrassing scenario due to the presence of white spots and white lesions. Children and parents are concerned about this unsightly appearance and often seek treatment to have these marks eradicated. White spot lesions (WSL) are defined as the enamel lesions that appear chalky white and opaque [1].
The white spot lesion has variable etiologies. It can arise from developmental cause such as fluorosis, molar incisor hypomineralisation. Defective maturation during amelogenesis can also results in WSL. This can be due to failure of the degradation and removal of some amino acid fractions or also due to trauma or death of maturing ameloblasts. Some ameloblasts recover from this insult resulting in varying degrees of opacities. Other causes include early caries lesion and post orthodontic demineralisation since fixed appliance therapy creates stagnation areas for plaque and make tooth cleaning difficult.
Adverse effects of these white spot lesions are that they may eventually lead to cavitation and their unaesthetic property affects the patient’s quality of life resulting in loss of self-confidence. A wide array of treatment options is available for aesthetic correction of white spot lesions. Minor defects may be managed with bleaching or micro abrasion, while severe defects need restorations, veneers, or full-coverage crowns. In case of pediatric patients, this is of major concern as the conventional treatment strategies for white spot lesion may require the use of hand piece and local anesthesia making the child anxious and fearful.
A new material for infiltration is an alternative therapeutic approach for masking these hyposcalcified areas. The goal of this treatment is to occlude the micro porosities within the lesion body by infiltration with low-viscosity light-curing resins that have been optimized for rapid penetration into the porous enamel [2]. ICON is an innovative product for the micro-invasive treatment of dental lesions on smooth surfaces.
Through this case series, we demonstrate the effective use of icon resin infiltration technique.
CASE REPORTS
Case No. 1
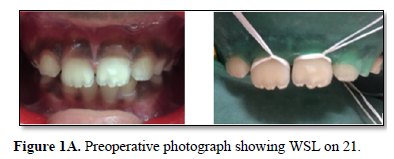
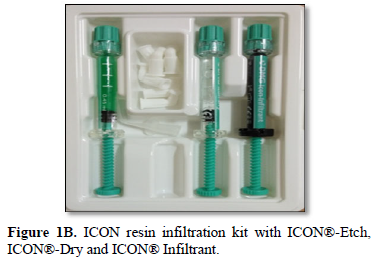
An 8-year old girl with a non-remarkable health history attended the Department of Pediatric and Preventive Dentistry, PMS College of Dental Science and Research for a routine examination and found the appearance of chalky white spot on her front tooth. Parents expressed deep concerns about this white spot. It is a moderate sized white spot lesion on upper left permanent central incisor (Figure 1 A). Different treatment options including resin infiltration, micro abrasion, resin restoration and benefits and risks involved in each treatment options were explained. Parents opted for resin infiltration technique. Tooth was cleaned with pumice using a rubber cup prior to the placement of rubber dam and resin infiltration was applied according to the manufacturer’s instructions. The tooth was etched with 15% hydrochloric acid gel (ICON® Etch; DMG, Hamburg, Germany) for 2 min to remove the highly mineralized surface and expose the lesion body followed by thorough rinsing with water for 10 s. Ethanol (ICON®‑Dry) was applied for 30 s and then air dried. The etching process was repeated two more times, followed by drying agent use. The infiltrant (ICON®‑Infiltrant) (Figure 1B) was applied to the tooth and allowed to penetrate for the next 3 min. The excess material was removed using an explorer and then cured for 40 s. Infiltrant was reapplied for 1 min, followed by 40 s of light curing. The tooth was polished with composite finishing burs. The white lesions disappeared. The patient and mother were very happy and satisfied with the treatment results (Figure 1C).
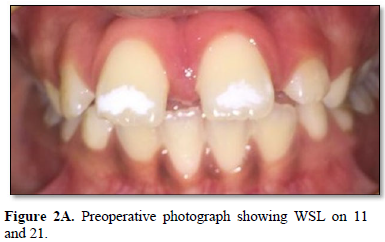
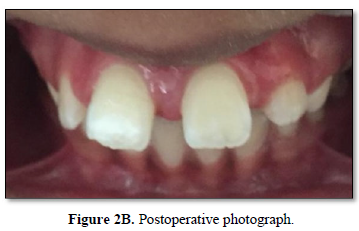
A 10-year-old boy with the known history of ADHD (attention deficit hyperactivity disorder) reported to our OPD with the complaint of diffuse white opacities on the 11 and 21 (Figure 2A). Patient was referred from nearby private clinic, as he was uncooperative for the treatment. The treatment alternatives with the risks and benefits involved were discussed with the parents and they opted to try resin infiltration and consented for treatment. Since this resin infiltration is a non-invasive option, patient was very cooperative, and treatment was carried out successfully. The WSL completely disappeared from 21 whereas in 11, opacity reduced to an appreciable extent. This difference in the treatment result may be due to the difference in the depth of demineralisation (Figure 2B). Both parents and patient were happy with the treatment outcome.
Case No. 3
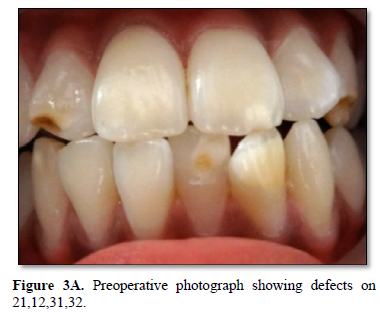
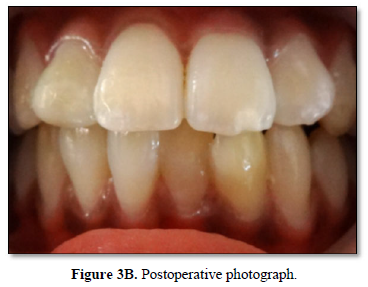
A ten year old boy and his parents reported to our OPD with deep concern about multiple white opacities on upper and lower anterior teeth. On examination it was noticed that WSL on 21,31,32 and frank cavitation on 12 (Figure 3A). The treatment options were explained to parents and they opted for resin infiltration technique. Since there were multiple opacities, parents opted to start with lower anteriors (31,32). Treatment was carried out with resin infiltration on 31 and 32, and cavities were restored with composite restoration (Figure 3B).
DISCUSSION
There is a dramatic change in the management of dental caries, from the traditional invasive restorative treatment approach to a more preventive approach, namely non-invasive or minimal invasive [3]. Instead of removing the porous carious tissue, at a relatively later stage, successful intervention to fill the micro porosities of the lesion at a much earlier stage with low viscosity light curing resins have been documented. This promising approach has been termed “resin infiltration” and has opened up an innovative way of treating initial carious lesions.
Enamel lesions are characterized by mineral loss in the body of the lesion, resulting in greater visual enamel opacity due to alteration of the refractive index of the affected area [4]. The characteristic chalky white surface of the lesion is caused by the increase in the internal porosities due to demineralisation, which results in loss of translucency. A sound enamel has refractive index (RI) of 1.62, while the micro porosities of enamel carious are filled with either watery medium (RI 1.33) or air (RI 1.0). The difference in refractive indices between enamel crystals and medium inside the porosities causes scattering of light resulting in a whitish opaque appearance of these lesions, especially when they are desiccated. The micro porosities of infiltrated lesions are filled with resin RI 1.46 which is more similar to RI of enamel and in contrast to the watery medium, cannot evaporate. The infiltration technique allows for reduction of the micro porosities (and therefore will hamper access of acids) and is capable of strengthening the demineralized tissue by mechanical support [5].
Various minimal invasive measures employed against WSL include oral prophylaxis, improved oral hygiene measures, use of remineralising flouridated (systemic and topical) and non-fluoridated agents. But these treatment regimens usually take longer duration and leaves behind unaesthetic ‘enamel scars’. According to Willmote [6], who studied the effect of fluoride after removal of fixed orthodontic appliance, stated that remineralization of white spots takes a long time, and the lesions may be left to some degree. And it can inhibit the mineralization of subsurface lesions. Contradictory to this, Ogaard et al. [7] warned against treating visible white lesions on labial surfaces with concentrated fluoride agents, since this arrests the lesion (hyper mineralization) and prevent complete repairs as deep lesions tend to remineralize only superficially. Consequently, arrested lesions show highly mineralized surface layers [8]. The underlying lesion body is still porous, and the whitish opacities often persists [9]. Moreover, during remineralization stains can be incorporated into the lesion, leading to the formation of brown spots, a situation that might be judged as even more unesthetic [8].
Enamel microabrasion was another method designed to improve the surface texture, remove the stains and improve the appearance of enamel. It removes superficial parts of the lesion by abrasion with a slurry of hydrochloric acid and pumice, and the enamel surface becomes smooth and glossy [8]. Comparing the effects of resin infiltration technique with microabrasion it was found that, is resin infiltration technique, only 30 to 40 μm are eroded in contrast with enamel micro abrasion with enamel removal is around 360 μm when applied in 5 s intervals and repeated 20 times [9]. Robinson et al. [10] reported that about 60 ± 10% of the lesion’s pore volume has been occupied by resin. According to Kielbassa et al. [11], resin infiltrates into subsurface lesions and produces resin infiltrated parts of the lesion and the depth of resin infiltration was over 100 μm. Unfortunately, resin infiltration technique could not remove white spot lesions completely in cavitated lesions and was later on corrected by composite veneer. The reason for some lesions being left after treatment could be that the depth of white spot lesion is not restricted to superficial part of enamel. It is reported the depth of resin infiltration is about 60 μm. If the depth of white spot lesion is deeper than 60 μm, it cannot be treated with resin infiltration technique. Therefore, caution should be taken in case selection.
CONCLUSION
The findings of the present case series prove that this minimally invasive resin infiltration of white spot lesion and caution should be exercised in case selection.
1. Mann NS, Makkar S, Gupta P (2015) Resin infiltration technique: The minimal invasive approach. TMU J Dent 2: 71-74.
2. Paris S, Meyer-Lueckel H, Kielbassa AM (2007) Resin infiltration of natural caries lesions. J Dent Res 86: 662-666.
3. Aoba T, Fejerskov O (2002) Dental fluorosis: Chemistry and biology. Crit Rev Oral Biol Med 13: 155-170.
4. Featherstone JD (2004) The caries balance: The basis for caries management by risk assessment. Oral Health Prev Dent 2: 265-269.
5. Paris S, Meyer-Lueckel H (2009) Masking of labial enamel white spot lesions by resin infiltration - A clinical report. Quintessence Int 40: 713-718.
6. Willmote DR (2004) White lesions after orthodontic treatment: Does low fluoride make a difference? J Orthod 31: 235-242.
7. Ogaard B, Rolla G, Arends J, ten Cate JM (1988) Orthodontic appliances and enamel demineralization. Part 2. Prevention and treatment of lesions. Am J Orthod Dentofacial Orthop 94: 123-128.
8. Ardu S, Castioni NV, Benbachir N, Krejci I (2007) Minimally invasive treatment of white spot enamel lesions. Quintessence Int 38: 633-636.
9. Tong LS, Pang MK, Mok NY, King NM, Wei SH (1993) The effects of etching, micro-abrasion and bleaching on surface enamel. J Dent Res 72: 67-71.
10. Robinson C, Hallsworth AS, Weatherell JA, Kunzel W (1976) Arrest and control of carious lesions: A study based on preliminary experiments with resorcinol formaldehyde resin. J Dent Res 55: 812-818.
11. Kielbassa AM, Muller J, Gernhardt CR (2009). Closing the gap between oral hygiene and minimally invasive dentistry: A review on the resin infiltration technique of incipient (proximal) enamel lesions. Quintessence Int 40: 663-681.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Journal of Allergy Research (ISSN:2642-326X)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Pathology and Toxicology Research
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)